Brooks: A Heart Hero’s Journey of Courage and Resilience
Written by Shannan & Jeremy
Brooks was born on July 23, 2018, at Women’s Hospital in Omaha. While we were aware that Brooks would be born with heart disease, the diagnosis quickly changed once he was born.

At our 20-week anatomy scan, we found out that the umbilical cord was a 2-vessel cord whereas a normal umbilical cord has 3 vessels. We were also told that they were unable to get enough pictures of his heart so they sent us to the Fetal Medicine Team at Women’s. On March 20, 2018, we went for our ultrasound and were told that they believed that Brooks would have Down syndrome and what they believed to be Tetralogy of Fallot. There were also a few items they mentioned regarding his stomach but to be honest, as soon as I heard something was wrong with his heart…I lost it. Did not hear another word and quite honestly, just wanted to run home and hide.
After the news settled, we went back to see the Fetal Medicine team for additional testing, scans, and a list of questions. At that time, we learned Brooks more than likely would not have Down Syndrome but they still believed he would be born with Tetralogy of Fallot.
We met with the surgery team and had several fetal echos to make sure everyone was prepared for what to expect after delivery. It was again confirmed that Brooks was what they were referring to as a “pink” Tet kiddo, meaning he would be born and his color would be that of a normal, Heart healthy kiddo, and we would take him home, monitor him until he was about 4-6 months old before he would need any surgical intervention.

Once Brooks was born, they were not able to stabilize him like they would with a TOF baby. Brooks was born at 4:30 pm and by 7:30 pm, he was being loaded into an ambulance and transported to Children’s Hospital. Dad followed Brooks to Children’s and once there, they began an entire workup to figure out why his oxygen wouldn’t stabilize. The following day, Dr. Fletcher informed us that while Brooks did not have TOF, he did have 4 different defects. He was diagnosed with a double aortic arch, atrial septal defect (ASD), ventricular septal defect (VSD), and bilateral superior vena cava. The double aortic arch had created a ring around Brooks’ trachea so anytime he would get worked up, that ring would tighten on his trachea and close his airway; therefore, he was intubated but it was in such a critical spot because the breathing tube had to be far enough past the ring but not so far that it entered his lung. Because of this, we were not able to hold Brooks. We did get special permission and a lot of assistance so that we could hold Brooks the night before surgery.
At 7:00 am on August 1, 2018, Dr. Hammel walked into the tiny corner room we were in and walked us through exactly what he planned to do to save our boy. Nothing can prepare you to hand over your 9-day-old baby for open heart surgery, but we did it with a TON of support from our family. After the longest 6 hours, we were told the surgery was successful and we could see our boy in recovery.
Brooks had a fairly easy recovery, and we went home on August 12, 2018. We spent 2 weeks at home, resting and recovering. On Sunday, August 26, we took Brooks to the ER because he refused to take anything by mouth and anytime he would cry or get upset, he would profusely sweat. They did a complete work up on him in the ER but ultimately determined his heart was functioning as expected and told us to follow up with his pediatrician the following day. On Monday, August 27, 2018, Brooks’ pediatrician admitted him back to Children’s due to his oxygen saturation. Dr. Duncan was waiting for us when we arrived in the PICU and completed a bedside echo. Everything looked great. They called in an ENT to do a bedside scope to check his airway and nothing was detected. At 3:30 am on August 30th, we received a call from the nurse that Brooks’ heart rate had dropped so they were having to give him breaths. We rushed up to the hospital and later that morning, he went back into surgery for a more in-depth scope of his airway. There they found a flap of granulation tissue which almost completely blocked his airway. Dr. Sewell clipped the tissue and from there on, we had a different boy. He could breathe without any noise and started eating like a little piggy. After a few more days of monitoring and one more scope to check for regrowth of the tissue, we discharged on September 4, 2018.
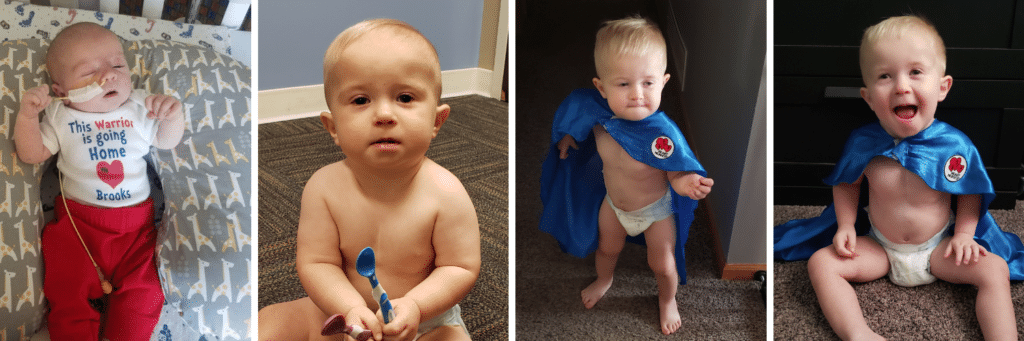
While the first few months of Brooks’ life were very eventful, he has remained mostly healthy with just a few hiccups along the way. He currently sees his Cardiologist every two years for an echo and EKG. He currently has a leaky aortic valve that they are monitoring.
We learned about Heart Heroes at one of our follow-up appointments with the surgery team. We received Brooks’ cape in time for us to participate in our first Superhero Heart Run in 2018. We have met several families that have become friends and have been able to participate in all the family fun events with Heart Heroes.
“We are honored that Brooks is being recognized as Heart Hero of the Month!”




