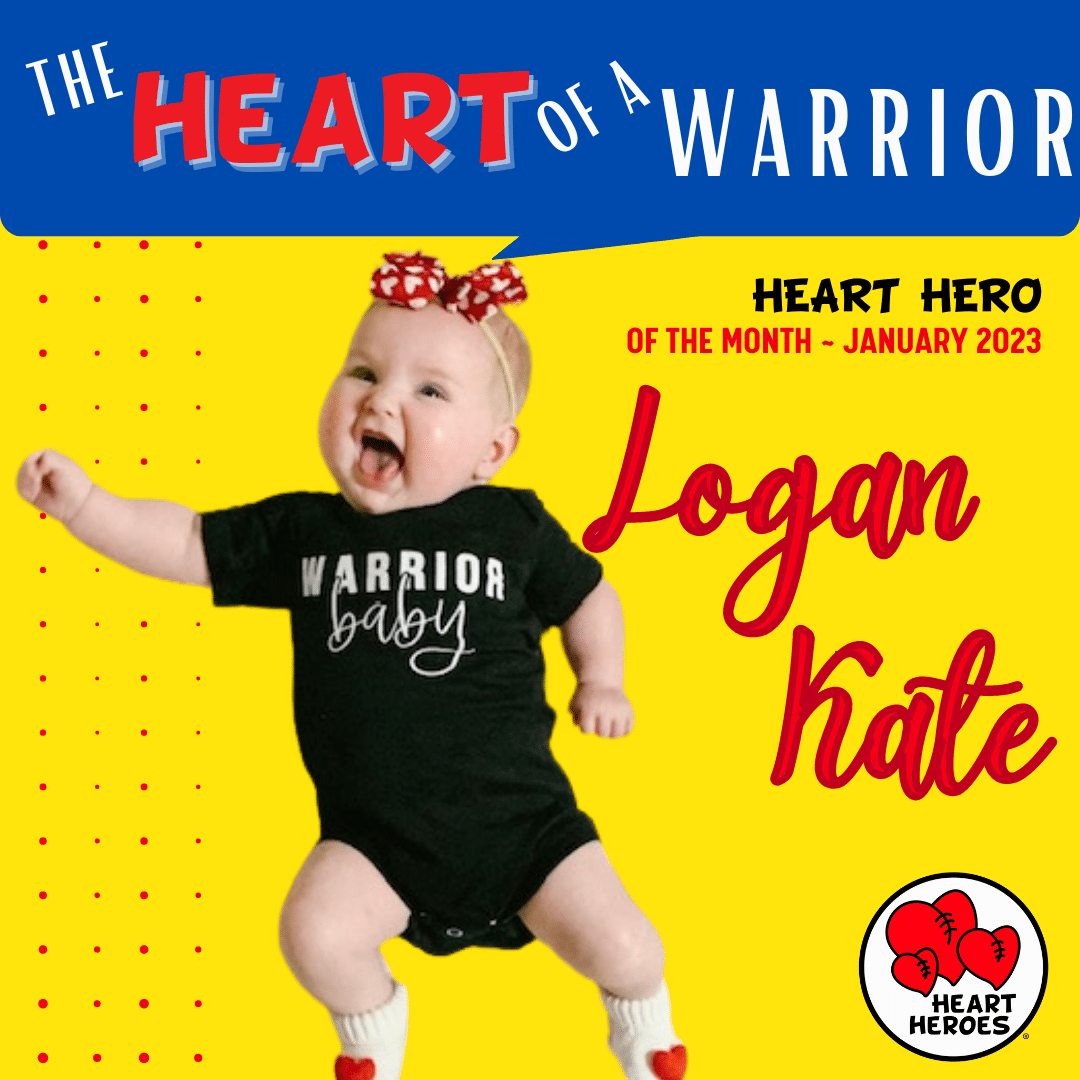
Heart Hero of the Month January 2023
Story by, ❤️Mom, Chelsea
On December 31, 2020, at our 19-week anatomy scan, it was discovered that Logan could have Congenital Heart Disease. At that time it was believed by my obstetrician that it was simply a ventricular septal defect (VSD) or possibly even only an error on the ultrasound. After a referral to a high-risk doctor and also Arkansas Children’s Hospital (ACH) cardiology department for fetal echocardiograms, it was confirmed that Logan not only had complex Congenital Heart Disease but a condition known as Heterotaxy Syndrome as well. During this time, I did more research than I have in my entire life. I read every peer-reviewed article I could find about Heterotaxy Syndrome and the different types as well as Endocardial Cushion Defect (which was the main known component of Logan’s defects). I looked into different hospitals to see where I felt Logan would receive the best care. I wanted to be as prepared as I possibly could be for Logan’s arrival. I would later learn that all the research in the world could not fully prepare me for the life of a heart mom and all the struggles and triumphs that title entails.

On May 12, 2021, Logan Kate Harmon was born. Our delivery went far better than we could have ever imagined. Because of Logan’s prenatal diagnosis, our delivery room was full of specialists prepared for the worst possible outcome. To everyone’s surprise, Logan was born pink and well-appearing. She was admitted to the Neonatal Intensive Care Unit (NICU) to undergo further diagnostic exams related to her Heterotaxy Syndrome. While Heterotaxy Syndrome itself is not a heart condition, it typically causes heart defects that vary in type and severity. Heterotaxy Syndrome affects 1 in 10,000 births worldwide each year. It is a condition in which the organs can be missing, misplaced, malformed, or multiplied. The most common organs affected by a diagnosis of Heterotaxy Syndrome include the liver, heart, lungs, stomach, spleen, and intestines. Each of these organs is affected for Logan. Logan has the left atrial isomerism form of heterotaxy. Logan has a midline liver, with complex congenital heart disease, both her right and left lungs have only 2 lobes, a right-sided stomach, multiple spleens that do not function, and intestinal malrotation. Logan’s first car ride was via ambulance from one NICU to another. Again, to everyone’s surprise, she absolutely thrived in the NICU and had a much shorter stay than originally anticipated. She was discharged to come home with her parents and big sister, Lainey, and to follow up with several specialists on an outpatient basis. Because she was doing so well, we believed we would have more time together as a family before Logan would need open heart surgery.

Not long after being discharged, we started to see the harsh reality that comes with complex Congenital Heart Disease. Logan was constantly sweating, breathing incredibly fast, had difficulties with eating, and would sometimes be blue. My husband and I would take turns trying to get Logan to eat around the clock. It would take her over an hour to eat 4 oz of formula. By the time she had finished a bottle, it was time for her to start on another one. Feeding continued to be a major struggle for Logan. She would gag so violently while trying to eat that the sound of her coughing and choking still haunts me. We discussed our concerns with her physicians.

To get a better understanding of the anatomical structure of Logan’s heart, it was recommended that she have an outpatient CT of her heart while sedated. During this procedure, Logan had a laryngospasm and her left lung collapsed. After she was extubated she was unable to keep her oxygen saturation in a normal range thus requiring supplemental oxygen. The original plan was an overnight stay in the Cardiovascular Intensive Care Unit (CVICU) with supplemental oxygen to let her rest and recover from difficult sedation. After her team of cardiologists and cardiac surgeons met, they felt it was in her best interest to keep her admitted until after her heart was repaired, which was tentatively planned for the same week. However, she ended up testing positive for RSV and Parainfluenza 3. Because of these lung infections, her team of doctors ultimately decided to delay her surgery for another 6 weeks to give her lungs time to heal before having open heart surgery. It was also at this time that it was decided to place a nasogastric tube (NG tube) as Logan’s sole source of nutrition. At that time, Logan was burning so many extra calories trying to eat by mouth that she was not growing like she should have been. Logan was discharged from the CVICU after being fully weaned off of supplemental oxygen.
Logan was able to stay home for about a month, but she continued to decline while we waited for her to reach her date for open heart surgery. During this time, she would have episodes in which she would become drenched in sweat, turn blue, and have no energy. Her oxygen saturation would be in the 60s/70s during these episodes. It was ultimately decided that we could no longer safely manage her symptoms at home, so we took her back to ACH to be admitted until after her repair. She continued to rapidly decline while inpatient. Her symptoms were worse than could be explained by her known defect. It was then decided to have a cardiac catheterization while an inpatient to better evaluate the pressures in her heart and lungs. Her team of doctors wanted to obtain as much information as they could before her surgery. Because Logan was so weak going into this procedure, they were unable to extubate her and she remained on a ventilator for the next 7 days. From her heart catheterization, it was learned that Logan had 5-6 times the amount of blood flowing through her lungs than she did to the rest of her body. Her lungs were essentially being flooded. At this time Logan was in heart failure and respiratory failure.

August 12, 2021: surgery day. We went into her room early that morning to try to spend time with her before having to hand her over for her life-saving surgery. She was wheeled back to the operating room at 7:45 A.M. The gut-wrenching feeling of her team of doctors taking her from us is one that I will never forget. To say we were terrified was an understatement. We knew that Logan was receiving the best care possible and never doubted their abilities, we just also knew that her life depended on this surgery. Because of COVID policies, only Kyle and I (Chelsea) were able to be present at the hospital for her surgery. We were isolated in a room by ourselves anxiously awaiting any updates on how her surgery was going while also trying to update friends and family who were praying for her. Logan’s surgery consisted of moving her right pulmonary veins and connecting them to the left side of her heart with a baffle and patching both her atrial septal defect and her ventricular septal defect. What seemed like an eternity passed and we were finally able to see our baby back in her room in the CVICU.

At this time Logan was experiencing a post-op complication known as junctional ectopic tachycardia (JET). Her heart rate was very high (up to 220s/bpm). Her care team worked to lower her heart rate with medications and also cooling her body. She was placed on an external pacemaker in an attempt to further regulate her heart rate. After 5 days of abnormal rhythm, Logan was finally in a normal sinus rhythm. Her pacing wires were kept in place for a few more days just as a precautionary measure. Logan had a few other minor post-op complications, but she continued to improve each day and her sweet smiley personality started to come back. After 1 month in the CVICU, Logan was discharged home again (still with an NG tube in place).

During this time, Logan was still having some symptoms of withdrawal related to medications she needed while she was hospitalized. She also had developed some oral aversions so we had to work diligently to be able to revert to oral feeds. We were finally able to remove her NG tube and go back to bottle feeding. Logan was still on multiple medications at this time so deciding to remove her NG was incredibly daunting. What if she started to refuse the medications that she still needs? What if she started to lose weight? What if she catches another virus? Logan surprised us and transitioned very well. Her biggest issue at this time is those common viruses (especially of the respiratory variety) have a much bigger and longer-lasting effect on Logan than most kids her age.
Thanks to genetic testing, her father and I learned that Logan’s condition was inherited from both of us. Logan has two changes in the MMP21 gene which causes Heterotaxy Syndrome in an autosomal recessive manner. Logan’s Dad and I (her mom) are both carriers of the mutated gene, and Logan inherited this mutation from both of us resulting in her expressing the mutation. To our knowledge, Logan is the only one in either of our families with this condition and she has been our only firsthand experience with congenital heart disease.


Our lives were forever changed the day we received Logan’s diagnosis. We appreciate things much more today than we previously did. We are very aware of how truly blessed we are to have Logan in our lives. Having a new baby sister is an adjustment for any 23-month-old big sister, but having a baby sister with complex medical needs is a whole different story. Lainey, our now 3-year-old, still has anxiety when Logan has to go to the hospital for routine doctors’ appointments. The love our girls have for one another is truly remarkable and something we prayed for every day since we even found out Logan would be joining our family. Logan’s Heart Hero cape is also something Lainey is very proud of. She is so proud to tell people about her “Sissy’s heart.”
Logan’s cape is hanging up in her room as a constant reminder of all of the things our baby has been able to overcome. She is truly our warrior and we could not be more grateful to call her ours.

Logan is now 20 months old and thriving. She has made her own timeline for development and has continued to amaze us with each new thing she learns and does. Her next cardiology visit is scheduled in 3 months where they will reassess her surgical sites and ensure that everything is holding up as it should. We are forever thankful to everyone who prayed for Logan and for the many, many people who have had a hand in her care.