It was just past midnight when I awoke to see a cardiologist performing an echocardiogram at the bedside.
How did we get here? Vincent had started the day not terribly hungry, and a little sleepy, but he was only eight days old and we had a big day with our newborn photos. Our pregnancy had been uneventful and delivery was a scheduled c- section at St. Francis Hospital in Richmond, VA. We were discharged home at four days old and fought some jaundice but that was all relatively normal newborn stuff. And yet, something felt wrong.
Earlier that day Vincent had been taken off of the Bili-blanket for his jaundice at home so we had an early afternoon appointment at the pediatrician to check his labs and progress with breastfeeding. When we arrived he seemed too quiet and too sleepy. Our lactation consultant, Laura Duke, is also a nurse practitioner and she listened to my concerns. She tried feeding baby Vincent with a syringe and the milk dribbled out of his mouth. We did skin- to- skin in office and when she returned I told her something just seemed off. I was a career Registered Nurse but worked with adults and had minimal knowledge about babies; however, my instinct told me we needed to take another look at Vincent. Ms. Duke listened to my concerns and took his temperature- it read 95 degrees. She continued to assess and calmly said she wanted us to go to the ER right away. Her initial thought was infection, so off went.
Upon arriving at the hospital the staff rushed us back and a team started working on our little guy. Suddenly, he looked so sick. How could we not know just how sick he was? What were we missing? The pediatric ER put him in a warmer and took blood cultures, urine cultures, and even did a spinal tap. We were taken to the “family room” and Vincent’s father, Raymond and I sat- so afraid. After the initial tests were completed in the ER we were admitted for IV antibiotics and further evaluation. We were met by Dr. Miller in the PICU. Dr. Miller was quiet and observed Vincent diligently. A few hours into our stay, he felt Vincent was breathing just a little too quickly, so he ordered a chest x-ray.
A chest x-ray is nothing too scary- I thought maybe he had pneumonia or a respiratory infection. After the x- ray was complete Dr. Miller came in and said, “Well, the x-ray of his lungs was clear but his heart looked a little enlarged so I am going to order an echo to have a better look”. Suddenly, this did not seem like normal newborn stuff. 1000 questions raced into my mind along with instant denial that nothing was wrong with Vincent’s heart. But Dr. Miller assured me we needed this out of “an abundance of caution” because “we did not want to think it was okay, we want to be sure”. At some point Raymond and I dozed off and awoke when the cardiologist began doing the echo at the bedside.
At this point, my nurse-brain was screaming “This is NOT normal”. In my career I do not think I ever saw a cardiologist come in the middle of the night to perform a test himself. We sat and stared at the screen while he did the echo- as if we knew what we were looking at- and heard him making side comments. Upon completion he conferred with Dr. Miller for what felt like hours.
Finally, Dr. Albrecht, the cardiologist with UVA Children’s Hospital at Richmond, returned to the room and asked us to be seated. He started explaining the anatomy of the heart, the challenges Vincent was facing, and that to fix Vincent’s broken heart he would need open heart surgery, immediately. And in that moment we joined a club no one expects to be part of- the heart parent club. The diagnosis, a Critical Coarctation of the Aorta. The fix, aortic advancement.
Just before sunrise on Vincent’s ninth day of life, we arrived on the seventh floor of the University of Virginia Hospital in Charlottesville, VA and were greeted by a team of residents, fellows, attendings, and nurses. A plan was discussed and his case was presented. Things were stable as he had been started on prostaglandins to maintain patency of the ductus- arteriosus and allow his little body to recover from the severe deprivation of oxygen his coarctation had caused.
Two days before Vincent underwent open-heart surgery we met the surgical director of pediatric congenital heart surgery at UVA, Dr. James Gangemi.
On August 31,
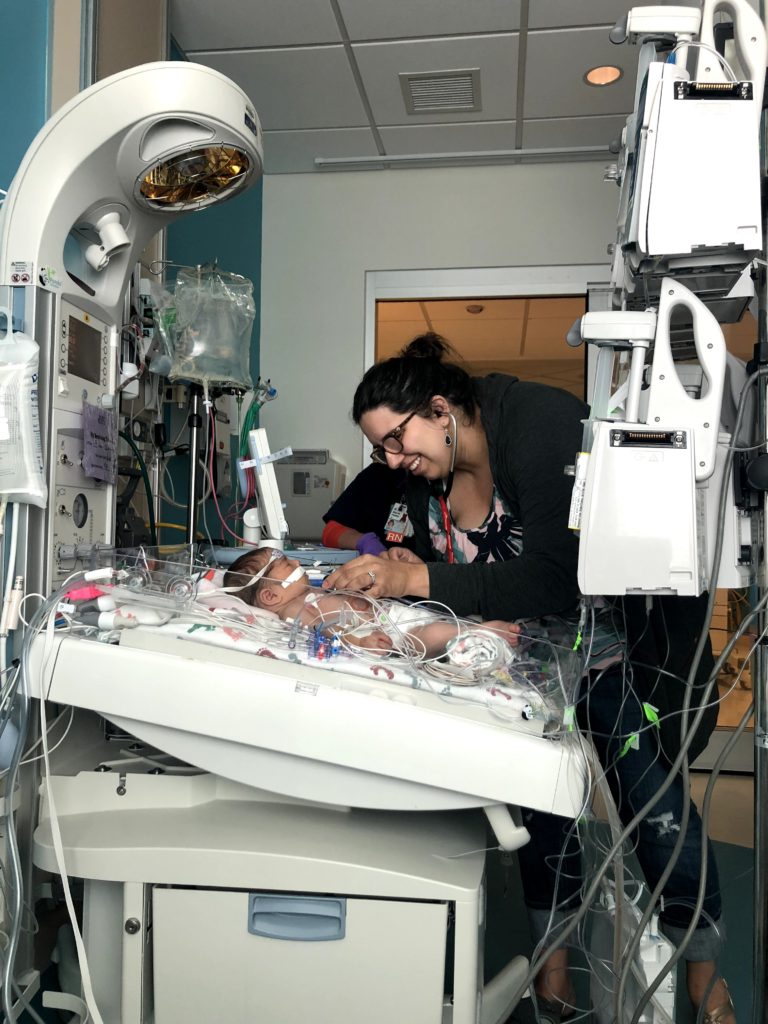
Recovery at UVA was filled with cheering for milestones we never knew we would want to reach. Vincent had specific parameters for blood pressure, heart rate, how much he could intake, how many minutes he worked with therapy, and every person we came in contact with helped him reach his next goal. Another week in the hospital, which flew by, and we were heading home. This would be our second first night home with a newborn and we were twice as nervous!
Following Vincent’s diagnosis and surgery we attended dozens of appointments and follow-ups and decided to embrace our status in the Heart Parent club. Through organizations like Heart Heroes & Mended Little Hearts of Central Virginia, we met wonderful people to give sound advice on how to be a heart parent and how to create an environment in which Vincent could thrive. All follow up echos have shown adequate flow through his aorta and his cardiologist, Doug Allen with UVA Pediatric Cardiology at Richmond, is very pleased with the surgical outcome.
At times, I grieve for the newborn days Vincent spent in the hospital fighting for his life; but this is just a chapter in his story.
He is a fighter and strong with a gentle spirit and full of joy.
For parents who may be new to the heart parent club or find themselves struggling with a diagnosis I fall back to the words of Bob Marley, “You never know how strong you are until being strong is your only choice”.